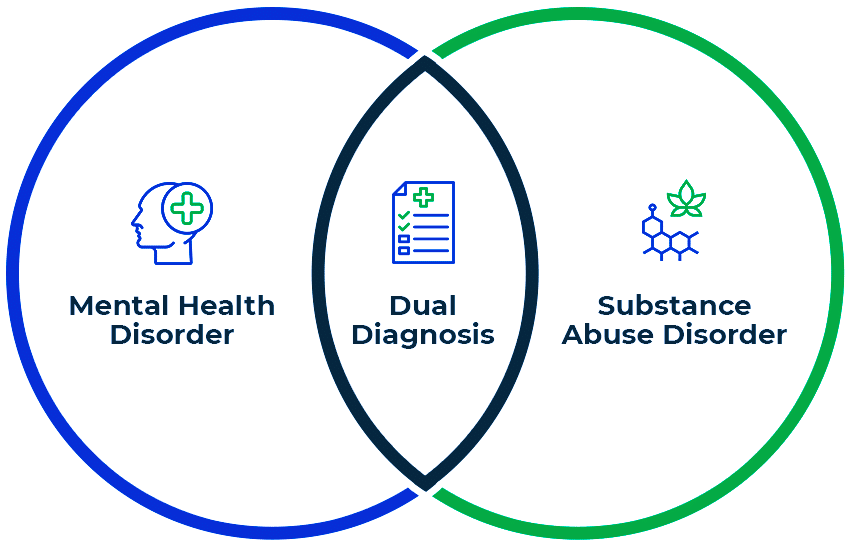
Dual Diagnosis
When a person struggles with both an addiction and a mental health disorder, this is commonly termed a dual diagnosis, or co-occurring disorder. The co-occurrence of mental health disorders and substance use disorders is fairly common. It can be difficult to identify if the substance use is the primary cause of the mental health disorder, or if it is aggravating the mental health disorder, or if the mental health disorder is primary and has contributed to the substance abuse.
Common Types of Dual Diagnosis:
There are several combinations of dual diagnosis, as there are many substance use disorders and many mental health disorders. Below are some of the most common forms of dual diagnosis:
Depression and Alcohol Use Disorder:
Depression frequently coexists with alcohol use disorder because alcohol can be used (and often is) to self-medicate symptoms of depression, which can lead to worsened depression with prolonged use of alcohol over time.
Bipolar Disorder and Substance Use Disorders:
Bipolar disorder has symptoms of depression and mania or hypomania in alternating patterns of time. Individuals with bipolar disorder also commonly experience substance use disorders, as many use substances to deal with the swings of their mood, or during mania to seek out euphoric experiences.
Post-Traumatic Stress Disorder (PTSD) and Substance Use Disorders:
PTSD can develop following exposure to traumatic events, and individuals with PTSD may use substances to cope with distressing memories, nightmares, or hyperarousal symptoms. However, substance use can impair the individual's ability to process and cope with trauma.
Schizophrenia and Substance Use Disorders:
Schizophrenia is a serious mental disorder characterized by hallucinations, delusions, disorganized thoughts, and impaired social functioning. Substance use disorders are often seen in individuals with schizophrenia, possibly as a result of attempts to cope with symptoms or cognitive deficits.
Borderline Personality Disorder (BPD) and Substance Use Disorders:
Borderline personality disorder is characterized by unstable moods, relationships, self-image, and impulsive behavior. Individuals with BPD often have comorbid substance use disorders, as individuals may consume substances to help cope with emotional dysregulation or feelings of emptiness.
Attention-Deficit/Hyperactivity Disorder (ADHD) and Substance Use Disorders:
ADHD is characterized by developmentally inappropriate levels of attention, hyperactivity, and impulsivity. Those with ADHD may be at greater risk for substance use disorders due to impulsivity, sensation-seeking behaviors, and difficulties with self-regulation.
Obsessive-Compulsive Disorder (OCD) and Substance Use Disorders:
OCD is characterized by intrusive thoughts (obsessions) and repetitive behaviors (compulsions). Individuals with OCD can have substance use disorders as a way to self-medicate anxiety associated with obsessions or compulsions.
Drug rehabilitation centers play a crucial role in the treatment of dual diagnosis, where individuals experience both a substance use disorder (SUD) and a mental health disorder.
Drug rehabilitation centers often have an integrated program that treats the substance use disorder and co-occurring mental health disorder(s) at the same time. The program sees the complexity of both conditions with programming that addresses all aspects of the person’s treatment.
Many drug rehabilitation centers have staff members with experience and training in treating dual diagnosis. The staff physician, psychiatrist, psychologist, therapist, counselor, and peer support specialists are trained to correctly assess and manage the substance use disorder and the mental health disorder.
Like other alternative rehab, our team will do a detailed assessment. This assessment determines the client’s substance use, mental health symptoms, medical history, psychosocial considerations, and treatment needs. This assessment will assist the team in developing an individual treatment plan for the person seeking treatment or their family.
Drug rehabilitation centers can offer different forms of psychotherapy and counseling to the person with a substance use disorder and the mental health disorder(s). Evidence-based therapies (CBT), dialectical behavior therapy (DBT), motivational interviewing (MI), and trauma-informed therapy help the person develop coping, management of cravings, address underlying issues, and prevent relapse.
Drug rehabilitation centers offer structure and support, reduce distractions and triggers, encourage healthy habits and self-care, and promote positive interaction with others. A sense of safety, stability, and accountability promotes recovery.
Drug rehabilitation centers help people with dual diagnoses establish aftercare plans and get connected to aftercare support services when they’re finished. Aftercare is the ongoing care that people are connected to after rehab, which can entail continued therapy, participation in a support group, medication management, job assistance, housing assistance, and other resources for recovery and avoiding relapse.
All in all, drug rehabilitation centers are critical to ensure that people receive systematic, specialized, and effective treatment for dual diagnosis. Drug rehabilitation centers treat both substance use disorder and co-occurring mental disorder(s) in a supportive, inviting, and therapeutic environment that empowers individuals to reach their full potential and enjoy a quality life of recovery.
- Feel free to contact us for more details
